Procedures, Vol. 1: Partial Splenic Embolization the First
It occurred to me as I was reading through my very inconsistent blog posts that there are probably (I think? tell me if you are!) a few CRC (colorectal cancer) patients and/or their caregivers reading my posts. It's always good to hear how other people got through something that you're afraid of or don't understand, so I've decided to start writing some mini "procedures" posts detailing my experiences with various tests, procedures, complications, chemotherapies, and so on. You can thank me (or throttle) me later.
Let's start with the fun one I just mentioned in my last post: the partial splenic embolization. Ever since I survived a rather significant surgical mistake during my liver resection in August of 2013, I've had problems keeping my platelet levels high enough to receive treatment. Chemotherapy, in its toxic quest to kill the fastest growing cells within the body (cancer cells), also kills healthy cells that grow quickly (hair, mouth cells, digestive linings, platelets, white blood cells, and so on). The trick is to find the balance that kills enough cancer cells without also killing the patient. In my case, the trick was to kill enough chemo cells but not so many platelets that I would be unable to continue receiving treatment.
This has been a tedious, consistent, frightening, laborious, unrelenting side show for the last 3 1/2 years I've been in treatment. Some weeks, my platelets were fine. Other weeks - no correlation to chemo most of the time, by the way - they were almost completely absent. We tried dose reductions. We tried waiting. We finally dropped the "ox" in Folfox for the last two of my post surgical chemotherapy sessions, in December 2013. And then I was NED! - for six weeks, upon which the whole carnival started up again. My platelets were trending in the 30 and 40k. Not enough to kill me (spontaneous brain bleeds can happen under 20K), but definitely not enough to allow treatment. We tried a new treatment, which worked well for me although I hated it with the burning hatred of 1,000 suns, but my platelets were still droopy. I received a compassionate use exception for a drug that can boost platelet production (sometimes). And that worked! - sometimes. I went to hematology, had several meetings with Dr. Hematology, who knew what she was doing but was a little old school because she was trained in East Germany (for reals). By old school, I mean that when it came time for them to extract bone marrow from my hip, I laid down on the table and she said, in an efficient German accent, "Your job is not to scream." Afterwards, once the needles were put away, I DID scream. She yelled at me, "We are finished! Why are you screaming now?" I said, "BECAUSE YOU TOLD ME I COULDN'T." Which basically sums me up in a nutshell, doesn't it? She determined that my bone marrow was making platelets (very good news), but she didn't know why they weren't out there doing their thang. The world's best heme/oncology fellow, Aaron, tried to figure it all out, for months. He did not succeed in doing so (still love you anyway, Aaron!). I took a chemo break and we tried our hand at SBRT (I owe you a post about that, too!), a targeted radiation surgicial therapy. Great results with it but it wasn't systemic treatment. I started maintenance chemo in May of 2015. Platelets did not like this development, but I got a fair number of rounds in me, all things considered.
Anyway. By early 2016, it was clear that something needed to change. My oncologist suggested a partial splenic embolization. They slip a catheter into an artery in your groin and guide it to the spleen. They release tiny microbeads or some kind of medical mousse/glue into a portion of the spleen, filling it up. Then they get the heck outta there. The portion of the spleen that's been filled is now unable to do anything and so that part dies - a painful death, I might add, as you'll see.
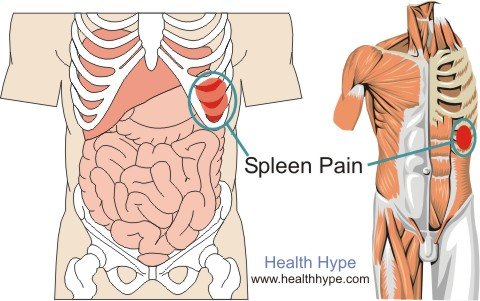
Not an actual picture of my spleen
My spleen on the scans had been looking "generous" for a while and at this point, it definitely looked much bigger than it should be. The theory was (and had been for a while) that my platelets were hanging out in there instead of circulating and doing their platelet duties. We do the embolization, the story went, and we'd have lots more platelets and a smaller, more manageable spleen. Sounds great, I said! Sign me up. Oh, by the way, they said, we have to make you aware of potential side effects. Yep, Yep, Okay, Sounds good. I signed until I reached one that said "pain syndrome" - ALERT. Uh, Dr. Sir? What's this? "Good question," he said. Up to 85% of people who undergo this procedure wind up with this pain syndrome. It shows up after about 5 days and requires lots of pain medication but then it goes away. Fair enough, I thought, as I finished signing. A little pain in exchange for platelets was an easy choice.
The procedure itself is about 1 1/2- 2 hours long, depending on a variety of factors. They keep you overnight for observation. I went in, got settled, was wheeled away, chatted with the peoples, they gave me the "twilight" versed and fentanyl combo that keeps you awake enough to follow directions but asleep enough that you can't feel anything. I was nervous. I don't like the twilight stuff (and I hate the book series, too - coincidence??) - because the first time it was used on me, I woke up to the news that I had advanced colon cancer and was in mortal danger. So, you know, a little skittish. This matters in practical terms because I stay awake for these types of procedures. Thus, I was awake for this procedure and remember vaguely seeing the little digital board that showed a bunch of pictures of my spleen from various angles. It was fascinating, really. So they finished mortally wounding part of my spleen (it takes several days for the affected area to actually die) and we zipped back to my little roomette (it was an overnight mini-floor for outpatient procedures - weird, huh?) and I came out of the twilight haze and felt...fine. Stayed the night (it was super quiet and nice and they didn't barge in and turn the lights on or anything at 3:30 in the morning; they just kept track of me via remote), and the next day I went home, took my regular pain meds as needed, and went about my business. Most of the week was great - I was up and around, feeling very sore but nothing terrible. And then.
AND THEN I HIT THE VAN WYCK.* On day five, I started to feel some pain. It was different from the soreness and overall achiness that lying around can bring. It started in the afternoon and by dinnertime, it had moved on to Some Pain. I doubled up on my pain medication and went to bed. This worked - until it didn't. Now, it was SOME REALLY BAD PAIN. The Pain Syndrome had arrived, and it did NOT creep in on little cat feet. IT SHOWED UP WITH A PLATOON OF SPECIAL OPS BAD GUYS SMASHING ME WITH BRICKS. It took my breath away. I literally could not breathe. Good thing I have supplemental oxygen, huh? (⛅ ← silver lining!) It was about 4:30 in the morning. We took stock. Too late to wake the neighbors and we hated to wake my mom, would have been there as zippily as possible but lives all the way across town, plus then we would have to wake the kids with the news that we were going to the hospital. No one likes surprises like that, expecially not small, somewhat anxious children. I didn't want to go to the hospital alone - I didn't think I could talk at all and needed my other half and my advocate. So, I curled up and breathed tiny little breaths and took more pain meds and had a heated wrap around my abdomen.
The children left for school. We raced to the hospital, calling my medical team on the way. The Emergency Dept at Univ of Colorado Hospital is extremely efficient, calm, knowledgeable, and interested in resolving your problem. This sounds like an obvious set of behaviors for a hospital ED to have, but it's not. I have been to several a bunch. They scanned me (I think?) but first they gave me medicine. Sweet, amazing, memory wiping pain killers. Eventually, I awoke. I was in a patient room. It took four days to get my pain under control. It was not a good time.
Oh, and the procedure? It didn't work at all.
So, what next? Of COURSE you know what's next. I DID IT AGAIN.
Sorry! Gotta run! But tune in next week and I will tell you all about it!
*This is only funny if you're a Seinfeld fan.


Comments
Post a Comment
Tell me...what are you thinking?